LARGE INCIDENTAL GASTROINTESTINAL STROMAL TUMOR OF THE STOMACH
Publikācija žurnālā Acta Chirurgica Latviensis Vol. 18 (1), 2020
Summary
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal neoplasms of the gastrointestinal (GI) tract (3). A 68-year-old male patient was referred to our hospital with complaints about feeling pressure in the thorax and heavy sweating for over 2 years. Abdominal CT showed a pathological formation approximately 21 cm × 15cm × 15 cm in size. The stomach was compressed and dislocated by the tumor. The total gastrectomy Roux modification was performed. The tumor grows from the back wall of the stomach; the tumor is not grew into the mucosa. We made a final diagnosis of an extra luminal GIST of the stomach – pT4N0M0G1R0 stage II. There was no evidence of disease recurrence six months after surgery.
Keywords: gastrointestinal stromal tumor, stomach, surgery
AIM OF THE DEMONSTRATION
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal neoplasms of the gastrointestinal (GI) tract (4). GISTs are more often located in the stomach (56%) followed by small bowel (32%), colorectum (6%), and esophagus (< 1%). Sporadically, it may affect the omentum, mesentery, and peritoneum (7). GISTs are usually found in adults between ages 40 and 70; rarely, children and young adults develop these tumors (3). We present case report of large GIST with non-specific symptoms. GISTs tend to displace adjacent structures rather than invade them, and because of their submucosal origin, they can reach large sizes before becoming symptomatic. As a result, surgical treatment become more difficult.
CASE REPORT
A 68-year-old male patient was referred to our hospital with complaints about feeling pressure in the thorax and heavy sweating for over 2 years. He lost 5 kilograms of weight in six months. During this time the patient was checked for the presence of cardiovascular disease. The abdominal cavity was not examined. There is no oncology history in the patient’s family. The holecistectomy was performed in 2008. Endoscopic examination of the stomach revealed no pathology in 2016.
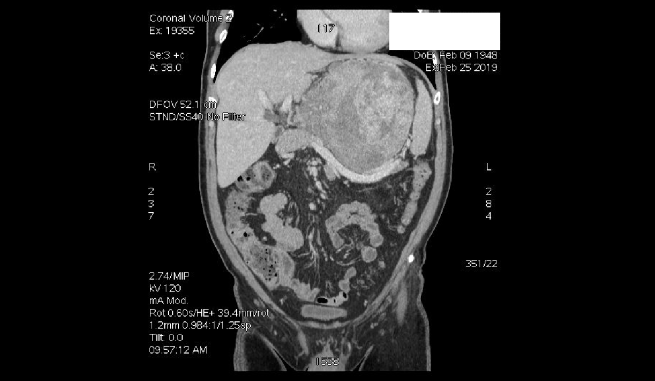
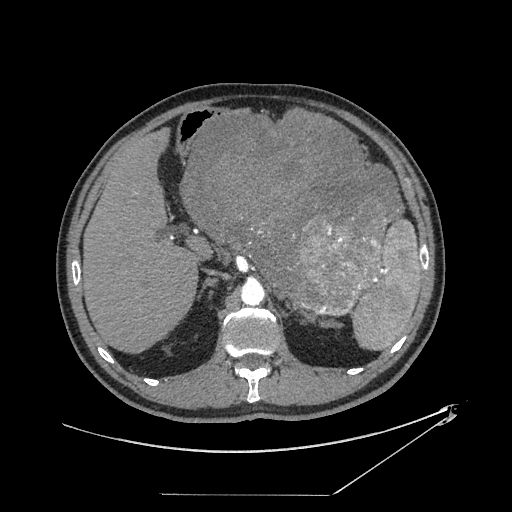
Physical examination showed tenderness in the mid and upper right abdomen. A mass was palpated in the upper abdomen under the sternum. The findings were otherwise unremarkable. Laboratory findings including blood chemistries, routine blood tests, coagulation profile, and tumor markers were normal. Abdominal ultrasonography revealed a smoothly contoured heterogeneous with good vascularisation mass, 20 cm × 14 cm in size. Abdominal CT showed a pathological formation approximately 21 cm × 15cm × 15 cm in size (Fig.1.). The tumor gets a blood supply from a. gastrica sinistra and a. lienalis. The stomach was compressed and dislocated by the tumor (Fig.2.). The pancreatic gland was flipped down by the tumor. The border between the back wall of the stomach and the tumor was indistinct (Fig.3.). Gastric endoscopy revealed external compression. The patient was prepared for surgical treatment. The total gastrectomy Roux modification was performed. The tumor grows from the back wall of the stomach; the tumor is not grew into the mucosa. It measured 22*15*21 cm in size and weighed 4.1 kg (Fig.4). Histopathological examination showed evidence of growth of spindle-shaped cells and a low mitotic index – <5/50 HPF. An immunohistochemical examination showed positive immunoreactions for CD34, CD117, but negative for cytokeratin. There were four lymph nodes in epiploon without metastases. Risk group of recurrence 3b – 12% (Miettinen and Lasota risk table for GIST). We made a final diagnosis of an extra luminal GIST of the stomach – pT4N0M0G1R0 stage II. The patient received parenteral nutrition because blood protein level was reduced after surgery. The post-operative course was without complications, and the patient was discharged on 14th postoperative day. Chemotherapy was not needed.
DISCUSSION
A high proportion of GISTs are asymptomatic. They are frequently discovered incidentally during an endoscopic study or on radiological images obtained for another purpose. Incidental findings can cause a significant diagnostic delay. Currently, a significant number of patients present with metastases at the time of diagnosis (up to 50% in some cases)(1). However diagnostic delay was approximately two years and the tumor was very large, no evidence of metastases in our case. CT is the imaging modality of choice for diagnosis and staging of GISTs at initial presentation and for monitoring the disease during and after treatment (9). Surgery is the only potentially curative treatment for suspected resectable GIST. The primary objective of this process is to ensure that clear resection margins are obtained in a complete resection of the tumor, and it can be extirpated without tumor pseudocapsule rupture (5). We performed total gastrectomy Roux modification with clear resection margins. The operation lasted ten hours. Surgical resection is the mainstay of treatment because adjuvant therapy is unproven. The surgeon should make every effort to achieve complete resection of all gross disease, which may necessitate the removal of adjacent organs (5;6). The low incidence of lymph node metastases confirms that lymphadenectomy is not routinely warranted (2). Recurrence of GIST is usual, and one report found only 10% of patients to be free of disease after long-term follow-up (8). No evidence of disease recurrence after six months in this case.
Conflict of interest: None


REFERENCES
Acta Chirurgica Latviensis (Latvijas Ķirurģijas žurnāls) ir zinātniskais žurnāls, kuru kopš 2000. gada izdod RSU sadarbībā ar Latvijas Ķirurgu asociāciju. Tajā ik gadu tiek publicēti oriģinālraksti, ārstēšanas rezultātu analizējoši pārskati, kā arī īsi klīnisko gadījumu apraksti, kas veltīti dažādām ar ķirurģiju un bērnu ķirurģiju saistītām nozarēm. Žurnāls veltīts plašai Latvijas topošo un praktizējošo ārstu auditorijai – speciālistiem, kuri ar ķirurģiskās ārstēšanas metodēm var palīdzēt pacientiem atgūt veselību.
2019. gadā žurnāls pie saviem lasītājiem atgriezās jaunā veidolā. Kopš 2001. gada žurnāls ir iekļauts arī Latvijas Zinātnes padomes vispāratzīto recenzējamo zinātnisko izdevumu sarakstā.